Why Human Leukocyte Antigens Are Essential to the Future of Medicine
At Orig3n, we’re working to drive advances in regenerative medicine that will make it possible for new tissues to be grown and organs to be repaired. Along the way, our researchers are always discovering new challenges that need to be addressed to make this vision a reality.
Human Leukocyte Antigens (HLAs) are one such challenge. To understand their role in the future of medicine, let’s start by talking about what they are and what they do.
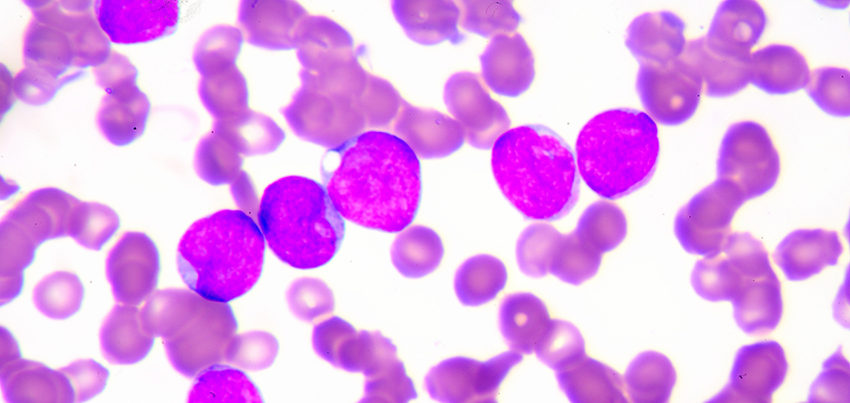
HLAs are a type of molecule found on the surface of most cells in the body. They’re composed of proteins, and are commonly called “markers.” HLA markers play an important role in immunity by helping the body tell the difference between its own proteins and foreign proteins, such as those found in viruses and bacteria. HLAs that your immune system believes are foreign to your body are flagged as substances that might harm you. It’s a protective mechanism that helps to keep you safe by activating your immune system when foreign substances are detected, which is a very good thing most of the time.
But those same protective factors can cause complications when you need an organ or tissue transplant.
Just as you have a blood type — one of eight possible combinations of A, B, and O plus Rh factors — you also have an HLA type. In the same way that you need a blood type match to successfully receive blood donated from another person without the immune system being turned against it, you need an HLA match to receive a successful organ, tissue, or cell transplant. If organs or cells from one person are implanted or administered to another person who has different HLA markers, they are instantly identified by the immune system as a threat and attacked, which is the last thing that patients want when they’re in desperate need of a new kidney, for example, or the cells they need to feel better. We at Orig3n are trying to solve this problem.
The challenge is that HLA matching is more difficult than blood type matching. There are so many possible combinations of HLA proteins that it can be hard to find a match that the body won’t identify as foreign.
The story of the world’s largest human blood cell bank
As we work to develop regenerative treatments — therapies in which we can grow tissue and repair organs using healthy cells — solving the challenge of HLA matching is high on our priority list. We know that success rates in organ transplantation and cell therapy procedures improve when there is a “deep match” between HLA types that reduce the likelihood of cells being rejected by recipients.
To do that, we built the world’s largest crowdsourced blood cell bank for regenerative medicine by collecting a teaspoon of blood from a large and generous group of altruistic people at events around the country. Each time that we collect a blood donation, we determine the HLA type of the cells. While most HLA-matching systems look for four to six HLA markers shared by the donor and the patient, we identify at least eight markers, which creates a higher likelihood of a “deep match.”
When we first started to build the cell bank, we intended to gather just as many samples as we needed to do our work. But then it grew. And grew. Now, after several years and many, many thousands of donations, there exists a huge repository of HLA-typed cells that can be used to develop cell therapies that are matched to the unique immune profile of the individual patient.
As Americans, we’re really lucky to live in a super diverse country, full of people from lots of different backgrounds and cultures. Much like our country, our blood cell bank has evolved into a snapshot of the entire world, including those of African, Asian, European and Latin American heritage. The bank now contains HLA matches for 90% of the U.S. population.
Today, we view ourselves as custodians of an immortal bank of cells. They’re not just helpful for us, they’re also an asset for humanity. Thanks to the depth and breadth of this blood cell bank, we’ll be able to grow cells of all kinds that match most HLA types. That can mean new heart cells to treat heart disease. Or liver cells to treat liver failure. Or cells that can be used to create a personalized treatment for a genetic condition.
It’s incredibly exciting. But we still need your help. While our cell bank matches 90% of people in the U.S., we want it to keep growing. The more samples we have, from more types of people, the more we can match and ultimately help. If you’re interested in learning more about our work — or donating your own blood cells to our bank — check this out.
Super HLA Donors
Similar to universal blood donors, HLA super donors can donate tissue and cells to more people without rejection — which increases our chances of developing treatments and therapies that will work for everybody. But super donors are super rare — about 1 in every 10,000 people.
When we started collecting these samples, we knew that statistically, we would find some of these super donors in our bank. And we have. One super donor may be able to contribute their cells to up to 6% of the population without rejection. Or 4%. This all depends on how common a particular super donor’s HLA profile is in the population. While a 2% match may not sound like much, it makes a big difference when you’re trying to find a match for everybody. The more super donors we find, the more matches we can make, which is why we keep collecting samples. Are you a super donor?!